Surgical Procedures for Primary GIST
This page describes the more common types of surgeries to remove primary gastrointestinal stromal tumors (GISTs). GIST Support International gratefully acknowledges the kind expert review of this material by surgical oncologist Christopher Windham, MD FACS. Dr. Windham heads the Florida Hospital Cancer Care Institute in Daytona Beach. You can read Dr. Windham’s tutorial Abdominal Anatomy for GIST in our website’s Ask the Professional section.
These are only general descriptions. The surgeon’s approach in an actual case depends on factors such as:
- the exact anatomical site of the GIST
- characteristics of the individual patient’s particular situation
- specific location of the GIST relative to the blood supply of the involved organ
- whether or not the GIST has adhered to, surrounded, or invaded adjacent structures
- the patient’s overall medical condition.
GIST can occur anywhere along the gastrointestinal tract (GI tract) from the esophagus to the anus, though the most common locations are the stomach (about 55-60% of cases) and small intestine (about 25-30% of cases).
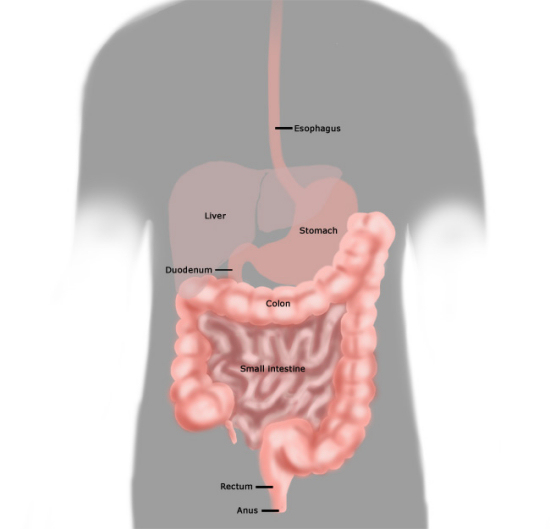
The Gastrointestinal Tract. Copyright 2010 by Margaret Stingley used with permission.
In most cases the GIST grows outward from the wall of the GI tract into the abdomen rather than growing into the interior of the digestive organs. This is in contrast to the common GI cancers (carcinomas) that grow inside the digestive tract from its lining tissues.
Esophageal Surgery for GIST
GISTs occur in the esophagus only rarely (perhaps 2% of GISTs). Other tumor types are more common in the esophagus. The esophagus presents a difficult surgical challenge due to its location beneath the breastbone (sternum), posterior to the heart and between the lungs. Sometimes a local excision or tumor enucleation may be used for a very small esophageal GIST. However, for larger tumors most of the esophagus is removed in an esophagectomy. The following diagram illustrates how the stomach is brought up through the space formerly occupied by the esophagus.
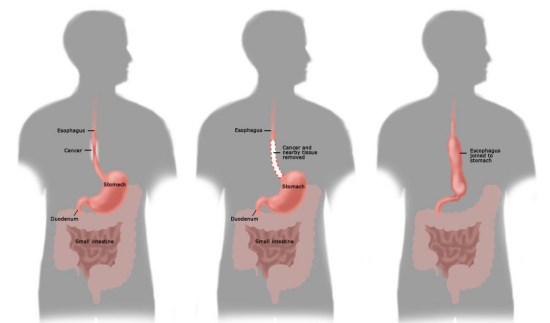
Normal esophagus (left) and esophagectomy. Copyright 2010 by Margaret Stingley (www.mstingley.com) used with permission.
Gastric Surgeries for GIST
-
The cardiac sphincter between the esophagus and the stomach: If this must be removed then the patient will have reflux from the stomach into the esophagus, especially if lying down too soon after eating a meal.
-
The pyloric sphincter between the stomach and the duodenum: If this must be removed then the stomach will empty quickly after eating, reducing both digestion and absorption of food in the stomach and potentially causing dumping syndrome, also called early gastric emptying.
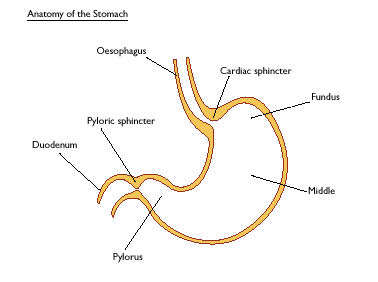
Lower esophagus (labeled oesophagus per British spelling) and the parts of the stomach. [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk ]
Wedge partial resection of the stomach
This may be done as an open surgery (laparotomy) or as a laparoscopic surgery. A wedge of stomach tissue containing the origin of the GIST is removed together with the tumor. The cut edges of the stomach where the wedge was removed are brought together and re-joined.&nnbsp; If the surgeon uses a stapler, the section of stomach to be removed (including the tumor) is pinched up, and the stapler is used to cut it out and re-join the edges in one step. Because only a portion of the stomach is removed, wedge resection does not require complex reconstruction
Billroth I partial gastrectomy, or gastroduodenostomy
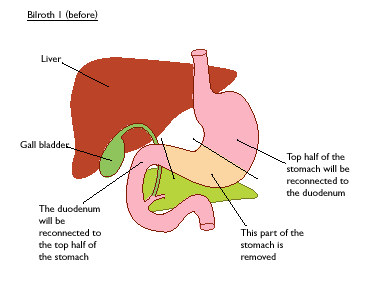
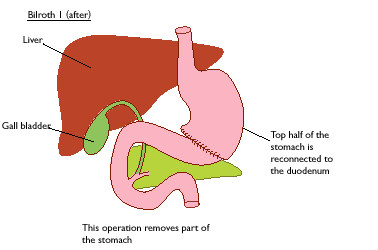
Billroth I Surgery: Before (top panel) and after (bottom panel). [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk ]
Billroth II partial gastrectomy, or gastrojejunostomy
In this surgery a variable portion of the lower stomach is removed, and the cut border is attached to the jejunum (small bowel) past the duodenum. The duodenum is retained to preserve the bile duct and pancreatic duct, but the bile and pancreatic enzymes do not meet the food to be digested until they flow from the duodenum into the jejunum.
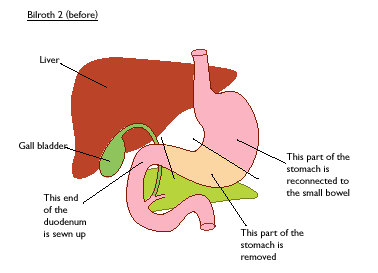
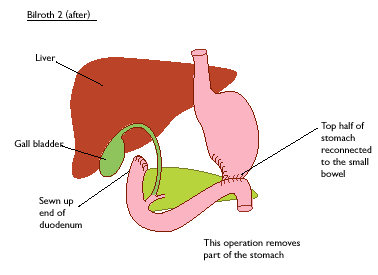
Billroth II Surgery: Before (top panel) and after (bottom panel). [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk]
Total gastrectomy with Roux-en-Y reconstruction
If the tumor involves the upper stomach or the gastro-esophageal junction then a total gastrectomy may be needed. In this case the esophagus is attached to the jejunum, as shown in the next figure. The disconnected duodenum is retained to keep the ducts through which bile and pancreatic enzymes enter the GI tract.
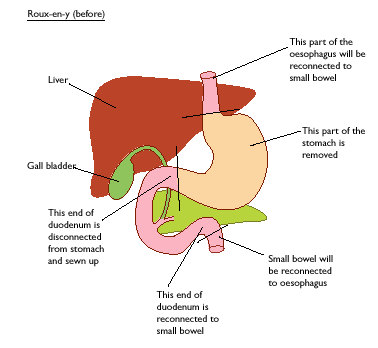

Roux-en-Y Total Gastrectomy: Before (top panel) and after (bottom panel). [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk]
Duodenal Surgeries for GIST
The duodenum is the first section of the small intestine; it is about 9 inches long, shaped in a distinct C curve around the head of the pancreas. It accepts partially digested food from the stomach through the pyloric sphincter. Additional digestive juices are secreted by the walls of the duodenum, further assisting digestion. Bile produced by the liver (to help digest fats) enters the duodenum through the bile duct from the gall bladder, which is an outpouching of the bile duct that acts as a reservoir for bile. Pancreatic digestive enzymes enter the duodenum through the pancreatic duct. The bile duct and pancreatic duct join together and enter the duodenum at a common point called the ampulla of Vater. The C-shape of the duodenum and the ducts emptying into it are shown in the next figure.
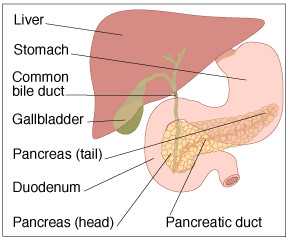
Anatomic relationship
of the duodenum and surrounding structures. [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk]
Partial Resection of Duodenum
Only about 5% of GISTs arise from the duodenum. If a GIST is small and is attached to a section of the duodenum far enough away from the ampulla of Vater, then it may be possible to perform a segmental resection of just the portion of the duodenum to which the tumor is attached.
Pancreaduodenectomy (Whipple resection)
For duodenal GISTs that involve the bile ducts or are very close to the ampulla of Vater, and for GISTs that are adherent to adjacent organs, a complex operation known as a “Whipple resection” or pancreaduodenectomy is needed. In this surgery the duodenum is removed along with the gall bladder, common bile duct, distal stomach, and the head of the pancreas. In some cases the surgeon can leave the entire stomach and pyloric sphincter intact (pylorus sparing pancreatoduodenectomy).
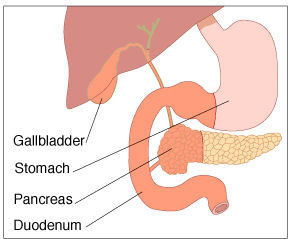
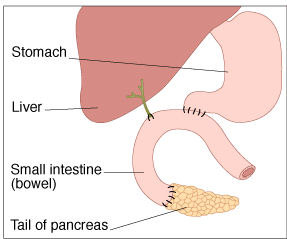
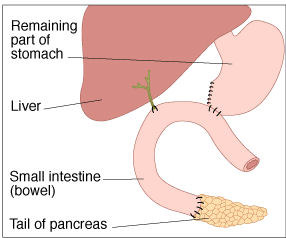
Pre-surgery anatomy (top panel) and pancreaduodenectomy either sparing the pylorus (second panel) or with resection of the pylorus (third panel). [Figure graciously provided by CancerHelp UK, the patient information website of Cancer Research UK, www.cancerhelp.org.uk]
Segmental resection of the jejunum, ileum, or colon for GIST
The small bowel (small intestine) and large bowel (colon) are where many nutrients are absorbed from digested food. The anatomical names duodenum, jejunum, and ileum describe the three successive sections of the single continuous tube that is the small intestine. Duodenal GIST was discussed previously. GISTs arising from the colon are rare (about 2%), but about 20% of GISTs do originate from the jejunum or ileum. The small and large bowels are essentially hollow tubes. Therefore, a segment where a GIST is growing may be removed and the cut ends reattached. Think of a leaky garden hose, and how you could cut out the bad section and then splice the remaining parts back together.
Surgery for rectal or anal GIST
Only about 5% of GISTs develop from the rectum and anus. The rectum serves as a reservoir for solid waste matter. This material is expelled when the anal sphincter relaxes to permit a bowel movement. A partial resection of the rectum may be used if a rectal tumor is not too close to the anal sphincter muscles. In this situation a temporary colostomy or ileostomy may be constructed to allow healing and minimize the significance of a leak (should one occur). A colostomy refers to the creation of a new exit for solid waste matter by routing the colon to exit the body through a surgically created opening (stoma) through the abdominal wall. A collection bag is attached to the stoma.
If removal of the upper rectum is required, the divided end of the colon may be connected to the remaining rectum at the time of tumor removal. Another option may include removal of the rectum and creation of a colostomy with the plan to return later to reconnect the bowel to remaining rectum or the anus, usually forming a pouch of colon tissue to serve as a substitute reservoir for improved bowel continence.
If the GIST is close to or involves the anal sphincter muscles, then an operation called abdominoperineal resection of the rectum (APR) may be performed. This involves removal of the anus and rectum. The end of the remaining sigmoid colon is brought out through the surface of the abdomen in a permanent colostomy.
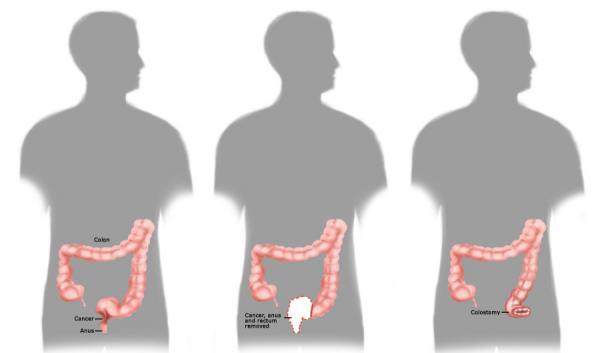
Abdominoperineal resection, showing colostomy. Copyright 2010 by Margaret Stingley, used here with permission.

