Abdominal anatomy for GIST: the peritoneum and retroperitoneum
 GSI asked questions about the abdominal membranes to Christopher Windham, M.D. Dr. Windham is a Surgical Oncologist in the Sarcoma Program of the H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida. He is an Assistant professor of Oncology and Surgery at the University of South Florida. His clinical practice is limited to soft tissue sarcomas with a special interest in retroperitoneal sarcomas. Dr. Windham has had his work published in several journals and has written a new text chapter about soft tissue sarcomas. You can view one of his papers online via the Moffit Cancer Center journal Cancer Control Here are Dr. Windham’s responses to GSI’s questions.
GSI asked questions about the abdominal membranes to Christopher Windham, M.D. Dr. Windham is a Surgical Oncologist in the Sarcoma Program of the H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida. He is an Assistant professor of Oncology and Surgery at the University of South Florida. His clinical practice is limited to soft tissue sarcomas with a special interest in retroperitoneal sarcomas. Dr. Windham has had his work published in several journals and has written a new text chapter about soft tissue sarcomas. You can view one of his papers online via the Moffit Cancer Center journal Cancer Control Here are Dr. Windham’s responses to GSI’s questions.
1. Can you explain the spatial and functional relationship of the peritoneum and mesentery to the abdominal organs?
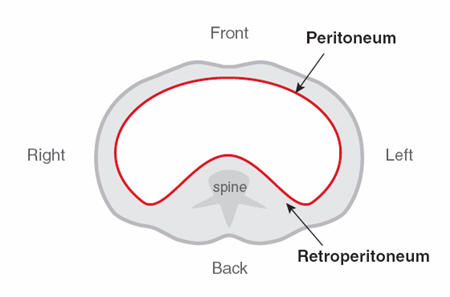
Visualize the abdomen as a completely empty shell. Let’s then imagine pouring a rubber substance that creates a continuous lining of this cavity. We will define this thin rubber liner as the peritoneum (Figure 1). In reality, it is a membrane just a few millimeters thick that has the ability to absorb fluids in the abdomen.
Now let’s imagine pushing this flexible lining inward, like pushing your finger into a balloon (Figure 2). This causes an indentation that is surrounded by the peritoneum, and the resulting double-layer structure is known as the mesentery, that encases and suspends the small intestine.
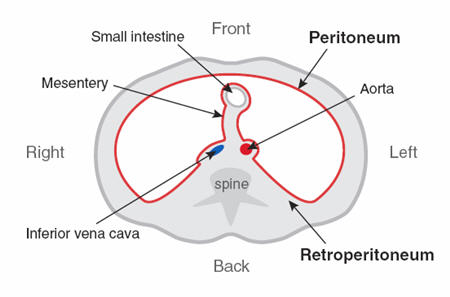
Figure 2. Mesentery surrounding small intestine. (Figure graciously provided by Christopher Windham, M.D.)
In between these peritoneal sides of the mesentery, we find fatty tissue, blood vessels and lymphatics that support the intestines (Figure 3). This is important in providing a healthy blood supply to the intestine and the return of nutrients absorbed by the gut to the circulation and lymph system. This in turn reaches your main circulation so the nutrients can be used to keep the person nourished. The mesentery also acts to anchor the bowel to the body. In this case the gut where the mesentery connects the bowel to the posterior muscular attachments.
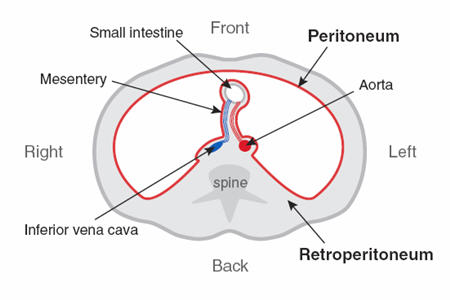
Figure 3. Mesentery with blood vessels serving the small intestine. (Figure graciously provided by Christopher Windham, M.D.)
We can now see the intraperitoneal and retroperitoneal regions. The area within the peritoneum is referred to as intraperitoneal. Before we begin to place organs within the abdomen, we need to clarify the boundaries of the abdominal cavity (Figure 4):
– Superior (closest to the head) is defined by the breathing muscle- the diaphragm
– Posterior (back) is defined by the muscles of the body wall and the spine.
– Lateral/anterior (sides/front)- are formed by the muscles of the abdomen
– Inferior (closest to the feet) boundary is formed by the muscles of the pelvic floor.
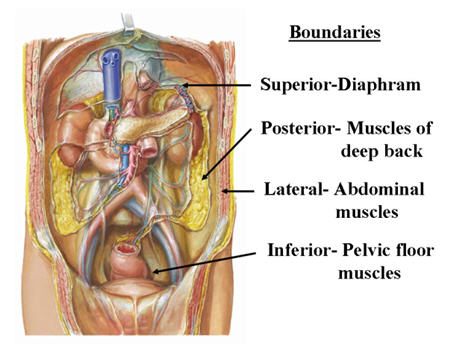
Figure 4. The abdomen viewed from the front of the body with the anterior chest and abdomen cut away. This view illustrates the boundaries and the retroperitoneal organs. Netter illustration used with permission of Elsevier Inc. All rights reserved.
Organs contained within the peritoneal cavity are called intraperitoneal and include the stomach, liver, gallbladder, most of the small intestine and a portion of the colon (transverse and sigmoid colon). Organs that lie behind these structures are referred to as retroperitoneal (Figure 5). These included the aorta (artery that carries blood from the heart to the body), inferior vena cava (vein that returns most of the blood from the body back to the heart), first portion of the small intestine (duodenum), pancreas, adrenal glands, the ascending and descending colon, kidneys, ureters (tubes that carry urine from the kidneys to the bladder), multiple sensory nerves to the abdominal walls (extending to the groin and upper legs), and nerves that regulate bowel control and sexual function (both found in the pelvic portion of the retroperitoneum).

Figure 5. Organ location with stomach, liver, spleen and most of the small and large intestine removed. Netter illustration used with permission of Elsevier Inc. All rights reserved.
With this background one should be able to define the peritoneum, retroperitoneum, mesentery, and locations of abdominal organs as related to their peritoneal locations.
2. Because the majority of GISTs arise from the stomach or small intestine, then they are intraperitoneal, right?
Yes. GISTs are usually found arising from the intraperitoneal stomach. GISTs can arise in the retroperitoneal portion of the small intestine (duodenum) and large intestine (ascending and descending colon).
3. We understand that GISTs most often metastasize to the liver or mesentery or peritoneum. Can metastasis be either blood-borne or the result of cells shed by the tumor?
Any malignancy may shed tumor cells within the peritoneal cavity resulting in tumor implants. The more common finding for GIST tumors is that of blood-borne metastases to the liver or direct extension of the primary tumor into surrounding organs. GIST tumors less commonly result in distant metastatic disease.
4. What GISTs are likely to be retroperitoneal, and how does this affect surgical intervention?
Very few GISTs would originate in the retroperitoneal space: as described above, retroperitoneal GISTs would arise from the duo
denum or from the ascending or descending portions of the colon. The impact on the surgery required would be dictated by what retroperitoneal structures/ organs are involved or are adjacent to the tumor. In general, a retroperitoneal location raises the complexity or the procedure and at times can result in the patient being deemed unresectable.
5. Why is it, if the duodenum is mostly retroperitoneal, that the Whipple surgery resects parts of structures that are intraperitoneal?
The Whipple procedure (pancreaticoduodenctomy) is a complex multi-organ resection usually employed for tumors arising in the duodenum and head of pancreas. This could be required for GIST arising in the duodenum, however the treatment of GIST rarely requires such a procedure. The reason for a Whipple resection is the blood supply; the head of the pancreas and the duodenum share their blood supply. Thus, if you try to remove just the duodenum, the head of the pancreas would not survive. This procedure also requires removal of the gallbladder, bile duct, and transaction of the pancreatic duct. Then the gastrointestinal tract has to be reconstructed as well as the bile duct and pancreatic duct.
6. Does the peritoneum safeguard the intraperitoneal structures from GIST arising in the retroperitoneum?
These tumors arise from cells within the wall of the gastrointestinal tract. The peritoneum is not a significant barrier to the invasive spread associated with malignancies.
7. Does the peritoneum at least provide a dividing line for “lifting away†a GIST from the surrounding normal structures?
At surgery this may in fact be the case, where the tumor separates readily from adjacent structures. However, GISTs are frequently found attached secondary to invasion. One of the difficulties we as surgeons face is knowing that information before surgery based on imaging studies. Experienced surgical oncologists usually proceed with the assumption that any structure touching the tumor may require removal. As such it may be necessary to be prepared to perform gastrointestinal, urologic, vascular and gynecologic procedures.
Figure 1. A slice through the abdomen showing the peritoneum lining the cavity. (Figure graciously provided by Christopher Windham, M.D.)

