Diagnosing GIST
What Is Needed to Diagnose GIST?
Usually gastrointestinal stromal tumor (GIST) is diagnosed from the features of the cells that comprise the tumor tissue with confirmation of the expression of the protein KIT (also called CD117) in the tumor cells, along with other proteins, by immunohistochemistry (a special laboratory technique to detect proteins in cells). In addition, certain proteins are very rarely expressed by GIST, such as desmin, and the absence of these proteins can also be useful diagnostically. Although a few other abdominal tumors can rarely test positive for KIT, the pathologist can use the results from a panel of tests to differentiate among the possible diagnoses. Those few GISTs that are negative for KIT can be identified by an expert pathologist using cell characteristics and the pattern of results for the panel of tests. Newer protein markers such as DOG1 (which stands for discovered on GIST 1) can also be helpful for diagnosis.
What is KIT (CD117)?
KIT protein (or CD117) is a cell-surface receptor for a growth factor called stem cell factor (SCF). KIT is a transmembrane protein: it straddles the cell membrane with a part extending outside of the cell (the extracellular domain) and a part extending into the interior of the cell (the intracellular or cytoplasmic domain). Normally, KIT triggers cell division, cellular differentiation, or other cellular functions when stimulated by stem cell factor.
 |
|
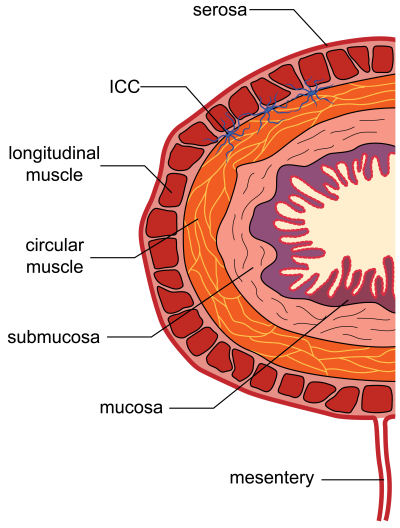
Figure 1. Cross-section showing the layers of the gastrointestinal tract. The ICCs are the stellate cells (shaped like stars) in blue (not to scale) residing between the longitudinal and circular muscular layers. These cells normally function to help mediate gastrointestinal motility (peristalsis). |
In the gastrointestinal tract, the KIT receptor is present on cells called interstitial cells of Cajal, or ICCs. These special cells control peristalsis, the GI tract movements that propel food along as it is digested. Because GIST cells show the same type of differentiation (or may even be derived from stem cells that produce ICCs), the tumor cells test positive for KIT in almost all GISTs.
The ICCs are located between the layers of the muscular wall of the GI tract. Note the figure illustrating a section of the GI tract wall. This could represent the wall of any digestive organ except the esophagus, which lacks the outermost serosal covering.
Common cancers (carcinomas) start from within the lining (mucosa) of the GI tract and often initially grow inside the digestive organs. In contrast, GISTs begin within the wall of the digestive organs (such as the stomach). At first the GIST is contained within the wall (called intramural), but as it grows larger it usually extends outward into the abdominal cavity. Occasionally a GIST may grow into the hollow tube of the digestive tract (called its lumen). Frequently GISTs ulcerate the lining at their point of origin and cause bleeding into the GI tract; this blood loss can cause anemia, but can also be the symptom that brings the GIST to the attention of the patient and their physician.
When was KIT first associated with GIST?
In 1998, Japanese researchers discovered that the presence of KIT protein distinguishes GISTs from other similar tumors, and that mutations causing the KIT protein to be abnormal are found in GISTs. Prior to that time, KIT testing was not performed and GIST was not always clearly recognized as a distinct sarcoma type. The consistent recognition of GIST became more common starting in 2000, and GISTs are well recognized by pathologists today. Before the discovery of KIT, many GISTs were thought to be a type of leiomyosarcoma, a sarcoma showing smooth muscle differentiation similar to the muscle layers of the GI tract.
Do KIT mutations cause GIST?
Yes, in the majority of GISTs, KIT is not only a marker that is helpful to identify GIST cells but also the initial factor responsible for the tumor’s development. KIT protein that is abnormally activated due to a mutation in the KIT gene causes uncontrolled cell division and tumor growth.
The growth factor called stem cell factor (also known as KIT ligand) binds two receptors at once and causes activation of the KIT receptor pair. When the growth factor locks into place between the exterior parts of two KITs to form a receptor pair (called “dimerization”), they change orientation and the portions inside the cell membrane come closer together. This allows each member of the pair to activate the other at an “activation loop” location inside the cell membrane. (The activation process is called “phosphorylation” because chemically this involves transfer of a phosphate group).
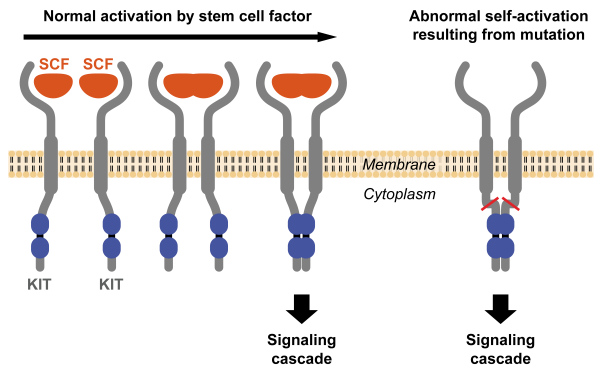
Figure 2. Two KIT receptors normally dimerize (form a pair) in the presence of the ligand stem cell factor (SCF) to initiate downstream signaling (left). Mutations in the receptor cause abnormal constitutive signaling without stimulation from the SCF ligand (right).
The activated KIT starts a series of signals to the cell nucleus, triggering the cell to enter the cell cycle and reproduce by cell division (called mitosis). By mitosis the single cell divides into two.
Normally in adults (who are no longer growing), new cells are not produced unless they are needed to replace cells that have been injured or have grown too old to function well. Our body organs stay a constant size because they maintain a constant number of cells. In a tumor, cells divide too often, causing the tumor to grow.
In normal ICCs, KIT triggers cell division only when a cell needs to be replaced. In contrast, in most GISTs, a mutation in the KIT gene causes the KIT receptors to signal abnormally for continuous cell growth, without being stimulated by stem cell factor. This uncontrolled growth causes a GIST to form. About 85% of GISTs are caused by a mutated KIT gene and the resulting malformed KIT protein that triggers abnormal cell division and tumor growth.
Other abnormalities of GIST cells that occur later in the tumor’s development also play a role in how aggressive the tumor becomes, but abnormal KIT activation is the primary cause.
Are all GISTs caused by mutations in the KIT gene?
No, there are two types of GIST with normal KIT protein:
PDGFRA-mutant GIST: About 5% of GISTs have normal KIT genes but are caused by an activating mutation in the gene for a different growth factor receptor called platelet-derived growth factor receptor alpha (PDGFRA). Normally, these PDGFRA receptor pairs join and signal the cell nucleus in just the same way as shown above for KIT, except that the growth factor that stimulates them is platelet-derived growth factor (PDGF). If the PDGFRA gene is mutated, then the protein PDGFRA can signal for continuous cell growth without being stimulated by PDGF, causing a GIST to grow.
Wild-type GIST: Tumors that do not have activating mutations in either the KIT or PDGFRA genes are called wild-type GISTs. Their growth triggers have not yet been
identified. These wild-type GISTs comprise about 10% of GISTs, including the majority of GISTs diagnosed in patients under 30 years old. As more research is done, this group will probably be divided into more subgroups with genetic abnormalities that have not yet been identified. A small number of these cases are already known to have mutations in the oncogene BRAF.
Do all GISTs test positive for KIT protein?
About 95% of GISTs are positive for the presence of KIT protein using immunohistochemistry. Almost all GISTs caused by a mutated KIT gene and almost all wild-type GISTs test positive for KIT. Some GISTs caused by a mutated PDGFRA gene test negative or very weakly for KIT protein when the pathologist stains the cells. It is not currently easy to test for PDGFRA staining directly because the commercially available reagents are not yet reliable enough for general use. A few specialized pathology labs may perform PDGFRA immunohistochemical testing. Alternatively, mutation testing of the PDGFRA gene may be recommended for diagnosis of KIT-negative GIST. While it is becoming increasingly used in GIST cases, mutation testing is not always part of a pathology report and some physicians are comfortable managing GIST patients without this information.
If the pathologist suspects that a tumor is a GIST but the KIT test results are weak or negative, then alternative tests can help identify the tumor type, as discussed in a later section on immunohistochemistry.
Is KIT testing always reliable?
The validity of KIT testing depends on the pathologist’s methodology and experience to avoid false positive results. Commercially available test materials are much more reliable now than they were in 2000-2002, when false positives occurred more frequently. If there is doubt, a tumor sample can be sent for a second opinion to a pathologist with more sarcoma expertise.
Is mutation testing needed for GIST diagnosis and prognosis?
No, mutation testing (also called genotyping) is not necessary for diagnosis of KIT-positive GIST, and it is not part of a typical GIST pathology report. Although some GIST treatment centers do routinely perform mutation testing on GISTs, this is not currently standard practice. Your pathologist may decide that mutation analysis is needed in the case of KIT-negative GIST, or if unusual tumor cell characteristics make diagnosis difficult. Your pathologist or your oncologist may decide that mutation analysis would be helpful in managing your treatment if there is reason to suspect an unusual mutation that would affect your response to drug therapies. Genotyping is done only in a limited number of labs; therefore, samples must be shipped for mutation testing unless you are being treated at one of the specialty centers with this capability. Regardless of whether genotyping is done locally or by an external lab, it will be reported separately, either as a subsequent addendum to your pathology report or as an entirely separate report. Also see questions 8-10 on the page GIST Pathology Questions and Terminology.
Go to next section, Pathology Methods for GIST

